Reversal of Skin Necrosis Caused by Facial Artery Occlusion

Full title: Reversal of skin necrosis caused by facial artery occlusion induced by a dermal filler using Platelet Rich Plasma.
Over the last several years, there have been more and more reports in the literature of vascular compromise caused by inadvertent injection of dermal fillers. Some of these adverse events may be caused by simple mechanical compression of a facial vessel but the most severe events seem to be a result of actual embolization of filler material into a facial artery resulting in vascular occlusion and subsequent necrosis of tissue supplied by the vessel.
There is scant information in the medical literature regarding how best to manage these difficult and potentially disfiguring injuries. Initial emergency treatment commonly consists of injection of hyaluronidase, topical application of nitroglycerine ointment, oral or topical antibiotics, oral corticosteroids, and sildenafil. Some physicians also advocate hyperbaric oxygen treatments.
This is a report of a patient who suffered from an arterial occlusion as a result of dermal filler injection and her subsequent course of recovery aided by aggressive use of Platelet Rich Plasma.
On January 18, 2016, a small amount of calcium hydroxyapatite was injected into the upper nasolabial folds of a healthy 35 year-old female. She reported no discomfort to her injector during or immediately after the injection. Within a few hours she noticed that the upper nasolabial fold area on the right and the corner of her lip on the right had turned a little darker. She also noticed some swelling inside of her mouth.
By the next day (Post Injection Day 1) she noticed an increase in the dark areas and an increase in the swelling inside her mouth. Also, the area was becoming a little painful. On Post Injection Day 2 she consulted with a dermatologist who injected hyaluronidase into the area and digitally massaged it. She also was started on topical nitroglycerine, sildenafil, cephalexin and prednisone (60 mg/day for 3 days, then 40 mg/day for 2 days, then 20 mg/day for 2 days). On Post Injection Day 3 she received a hyperbaric oxygen treatment for 45 – 60 minutes.
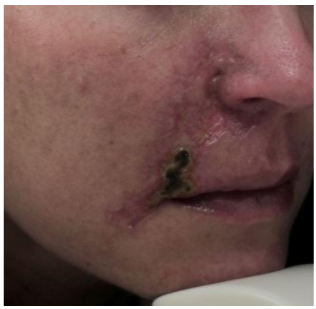
On Post Injection Day 5 the patient took the photo below 5 with her cell phone.

Post Injection Day 5
On Post Injection Day 8, she received a second hyperbaric oxygen treatment. On Post Injection Day 9, she came in to see the author who initiated a Platelet Rich Plasma treatment program. The photograph below was taken by the author on Post Injection Day 9 or Treatment Day 0 (TD 0).

PID 9, TD 0
Since the previous photograph, there had been some minimal improvement in the dark necrotic area above the right naris and below the right commissure and some minimal re-epithelization. There was no necrosis or discoloration inside the mouth but there was still a dark necrotic appearing eschar along the nasolabial fold to the lip. The author administered her first treatment with Platelet Rich Plasma (PRP) on TD 0.
Approximately 10 cc of blood was drawn into an 11 cc PRP Tube and spun for 12 minutes to separate the red blood cells from the platelets and plasma. Approximately 7 cc of plasma were obtained. Approximately 3 cc of platelet poor plasma supernate was discarded and the platelets in the remaining 4 cc of plasma were re-suspended to produce a super-concentrated PRP suspension. Calcium gluconate 0.6 cc was added to activate the platelets. Several injection sites were chosen and cleaned with betadine. Approximately 3 cc of the PRP was injected under the affected areas with a 30 G needle and the remainder was dripped onto the raw skin surface and massaged into the tissue. The patient was advised not wash her face for a few hours to allow the PRP to seep into the raw skin.
Two days later, on TD 2, she returned for follow-up. In the interim, she had received one additional hyperbaric oxygen treatment. The photograph labeled TD 2 was obtained.
TD 2
On TD 2, the epithelial borders were felt to be still too fragile for the mechanical trauma of microneedling so the PRP injections and topical application were repeated as before with the intention to eventually progress to microneedling to enhance the absorption of the PRP.
The patient returned on TD 6 and in the interim, had received an additional hyperbaric oxygen treatment. The PRP injections and PRP topical application were repeated as before.
She returned on TD 9 and in the interim, had received yet another hyperbaric oxygen treatment. On TD 9, the epithelial borders seemed to be healthy enough to support microneedling. As before, approximately 4 cc of super concentrated PRP were extracted. A small amount of anesthetic cream was applied to the epithelial edges with a Q-tip. Microneedling was performed at a depth of 1 to 1.25 mm. Three cc of PRP were dripped directly onto the microneedled areas and gently massaged in. One cc of PRP was injected along the epithelial borders superficially.
She returned on TD 14 after having received another hyperbaric oxygen treatment. The photograph labeled TD 14 was taken. She had received a total of five hyperbaric oxygen treatments and four treatments with PRP one of which included microneedling over a two week period. The necrosis had nearly completed resolved.

TD 14
The hyperbaric oxygen treatments were stopped but she continued to receive PRP injections and microneedling treatments at gradually increasing depths on TD 14, 20, and 28. The photograph labeled TD 40 was taken 49 days after the injury and 40 days after PRP treatments were initiated by the author.
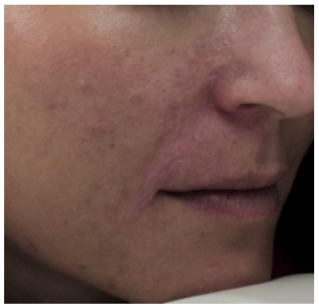
TD 40
Although the necrosis had completely resolved, the patient continued to receive monthly PRP treatments to improve the texture and to soften the edges between the damaged and undamaged areas. Pre-treatment with a roller Radio Frequency device was added to stimulate additional collagen production before each PRP treatment. The patient felt that the Radio Frequency treatments helped accelerate improvement in texture.
CONCLUSION and DISCUSSION:
Inadvertent intra-arterial injection of dermal filler is likely to be significantly more common than reported in the literature. Aspiration prior to injection is recommended by filler manufacturers but most of the commercial fillers are not designed to display a flash of blood when the syringe plunger is pulled back. It can be very difficult to determine whether or not there is intravascular placement of the needle tip prior to injection. Also, usually these patients do not experience adverse symptoms from intravascular placement of filler until hours later. Phone calls from patients experiencing post-injection symptoms should be taken very seriously.
The use of injected hyaluronidase for emergency treatment of vascular embarrassment from dermal fillers has been recommended by several experts even if the filler causing the vascular compromise is not hyaluronic acid but calcium hydroxyapatite. Injected hyaluronidase may be effective at dissolving hyaluronic acid filler putting direct pressure on a vessel from outside its lumen. Presumably some hyaluronidase may possibly even penetrate into an occluded vessel to dissolve intravascular hyaluronic acid.
It is difficult however to understand how hyaluronidase would help relieve pressure or embolization from an injection of calcium hydroxyapatite, a filler which can not be dissolved by hyaluronidase. It is possible that hyaluronidase injected into an area of vascular occlusion or compression as a result of injection of calcium hydroxyapatite may even cause loss of some the patient’s native hyaluronic acid resulting in a volume defect that will require subsequent correction. Additional research would help clarify these points.
To date, there are no widely accepted treatment protocols to treat the necrotic aftermath of vascular compromise from dermal filler injections. I have seen and reported here rapid and dramatic improvement in facial necrosis by the aggressive use of Platelet Rich Plasma both directly injected and topically applied after microneedling. Physicians with patients who present with this dramatic complication may wish to employ aggressive PRP therapy prior to resorting to surgical debridement and repair.
PRP treatments may also be considered in other aspects of wound care. Diabetic ulcers, pressure sores, deep traumatic abrasions, and thermal injuries may benefit from vigorous treatment with PRP.
October 13, 2016
Francis E. Toscano, M.D.
Medical Director, Red Bamboo Medi Spa
2516 C McMullen Booth Road
Clearwater, FL 33761
727-432-7286
ftoscano@redbamboomedispa.com